A 60 year old man resident of Nalgonda weaver by occupation came with
CHIEF COMPLAINTS :
*PEDAL EDEMA from 6 months
*Decreased urinary output since 1 month
*Vomitings since 10 days
*Sob and facial puffiness since 2 days
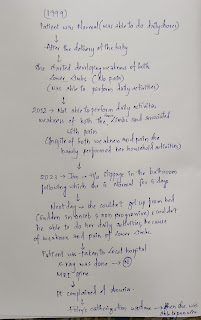
HOPI:
Patient was apparently asymptomatic 6 months back then his creatinine was 3 mg/dl and was diagnosed with chronic kidney disease. Since 1 month he is complaining of decreased urinary output
C/o vomitings since 10 days,non projectile,food particles as content,non bilious,non blood tinged
C/o SOB since 2 days grade 2 and relieved by taking rest
C/o facial puffiness since 2 days
PAST HISTORY:
Patient is known case of Chronic renal failure
:6 months back.
*K/c/o DM since 15 years and on Inj mixtard
20U-x-8U
*He is a known case of hypertension for which he is on Amlong 10 mg
K/c/o TB - 2 years back
FAMILY HISTORY:
No relevant family history .
*PERSONAL HISTORY :
DIET :mixed
APPETITE:Normal
SLEEP: Inadequate
BOWEL AND BLADDER : Decreased urine output since 1 month and normal bowel movements
ADDICTIONS: Drinks alcohol occasionally stopped since 5 months
GENERAL EXAMINATION:
Patient is conscious, coherent and co operative and the patient is moderately built and moderately nourished
Pallor: absent
Icterus:absent
Clubbing: absent
Cyanosis: absent
Lymphadenopathy: absent
*BILATERAL PITTING PEDAL EDEMA +
*VITALS :
*TEMPERATURE:98°F
*BP :150/70 mmHg
*PULSE RATE :84 bpm
*RESPIRATORY RATE :22 breaths per min
*SYSTEMATIC EXAMINATION:
*CVS :S1 and S2 heard and no murmors
*RS :
•Dsypnoea: -
•wheeze: -
•Trachea : centrally placed
•chest is normal
•Bilateral air entry present
*ABDOMEN :
∆Shape of abdomen: distended
∆Tenderness : No
∆palpable mass : No
∆Liver : Not palpable
∆Spleen : Not palpable
*CNS : No focal neurological deficit.
Investigations:
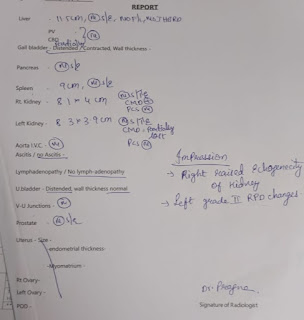
USG
Provisional diagnosis:
AKI ON CKD
DYSELECTROLYTEMIA (HYPOKALEMIA AND HYPONATREMIA)
TREATMENT:
1) FLUID RESTRICTION <1 L/DAY
2) SALT RESTRICTION<2 gm/ day
3)INJ ERYTHROPOIETIN 4000IU SC / ONCE WEEKLY
4)INJ HAI SC /TID
INJ NPH SC /BD ACCORDING TO GRBS
5) TAB NODOSIS 500 MG PO/BD
6) TAB OROFER XT PO/OD
7) TAB SHELCAL CT PO/OD
8) TAB AMLODIPINE 10 MG PO/OD
9) INJ MONOCEF 1g IU /BD
1-X-1.






Comments
Post a Comment