A 25 YEAR OLD MALE PATIENT WITH YELLOWISH DISCOLORATION OF EYES AND URINE, ABDOMINAL DISTENSION AND SOB
A 25 year old male who is a resident of yadagirigutta Mason by occupation came to casualty with chief complaints of :
*DISTENSION OF ABDOMEN SINCE 6 DAYS
*SHORTNESS OF BREATH SINCE 6 DAYS
*YELLOWISH DISCOLORATION OF EYES AND URINE SINCE 6 DAYS
•HISTORY OF PRESENTING ILLNESS :
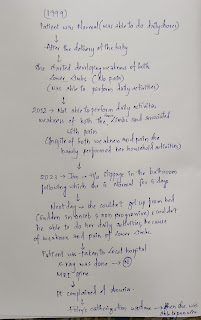
Patient is apparently asymptomatic 3 months ago he then developed abdominal distension which is insidious in onset and gradually progressive associated with shortness of breath 3 months back which is of grade 2 and it progressed to grade 3 over 3 months .He also has yellowish discoloration of eyes and urine 6 days back .He also has similar complaint 4 months ago for which he took herbal medication for a week and the symptoms subsided and he also stopped drinking for 7 days after that he continued drinking .He also complaints of fever 3 months back which is intermittent which is not associated with chills and rigors for 2- 3 days And cough which is non productive 10 days back .
Vomiting 2to 3 episodes per day which is non bilious, which contains food and water as contents.
There is increased facial puffiness and pedal odema which is of grade 2 which subsided after medication .
He also complaints of palpitations and altered sleep cycle.
He also has delirium 7 days back it continued for 1 day .
Ascitic tap is also done on 29/ 07/22 .
DAILY ROUTINE :
He usually wakes up at 7 in the morning and do his daily routine work without consuming food or any breakfast he will go wine shop and consumes alcohol (90ml 2-3 bottles along with thumbs up and afternoon he repeats the same and in the evening he will take some fruits or coconut water because of his mother's pressure and at night we will again take alcohol 90 ml (2-3 bottles) and he goes to sleep barely he takes any food .
PAST HISTORY:
A 25year male had complaints of fever and vomiting 3 months ago, for which he sought for consultation and diagnosed to be having liver disease and jaundice. After 15 days of treatment, the clinical manifestations were resolved. He started drinking 360ml of alcohol per day, after resolution of Symptoms for a month. Then he had symtoms of abdominal distention, pedal edema and yellowish discolouration of eye for which he used herbal medication; the symtoms resolved in a week. He again started drinking alcohol and toddy along with herbal medication, he stopped alcohol for 2 days, because of lack of money, he had symtoms like aggitation, irritability and visual hallucinations; resolved after having alcohol. 2 days ago he had similar hallucinatory symtoms. His last binge was on 24/07/2022.
FAMILY HISTORY :No similar complaints in the past .
PERSONAL HISTORY :
*DIET:MIXED
*APPETITE: DECREASED
*SLEEP: INADEQUATE
*BOWEL AND BLADDER:
-GREEN COLORED STOOLS 7 DAYS BACK ( 3-4 TYMS)
-ANURIA ONE WEEK BACK ( ONLY ONCE A DAY)
ADDICTIONS:
Smoker since 10 years; initially he used to smoking 3-5 Cigarettes per day which has been increased to 10 Cigarettes per day; during treatment he used to smoking 2 -3 Cigarettes per day.
Alcoholic since 10 years; initially 160ml per day for 3 years which was increased to 240 -360ml per day depending upon the availability of money.
From past 5 months he stopped going to work due to health issue and dependent upon his wife.
He was beaten up by someone in the Left chest for which he was having pain; drinks alcohol to reduce that pain.
GENERAL EXAMINATION:
Patient was conscious, coherent, cooperative poorly bulit and moderately nourished
Pallor- cannot be examined due to Yellowish discoloration.
Icterus- present
On 30/07
cyanosis: Absent
Clubbing: absent
Generalised Lymphadenopathy: Absent
Pedal edema : absent
Vitals:
Temperature
Heart rate:94beats/ min
Blood pressure:118/76 mmHg
Respiratory rate:19 cycles/ min
SYSTEMIC EXAMINATION
Abdomen :
Soft and non tender, Distended.
Inspection: Abdomen distended
No scars,sinuses.
Umblicus inverted
No dilated veins
Palpation: All inspectors findings are confirmed Abdomen is soft and non tender
No visible pulsations
Hepatomegaly
Spleen
Percussion:
Resonant note heard
Shifting dullness present
Auscultation:
Bowel sounds heard.
Respiratory system:
Inspection:
Shape of chest:Barrel shaped
Gynaecomastia present
A scar present over the rt side
Trachea : central
Wheeze is heard
Palpation:
All inspectors findings are confirmed by palpation
Chest movements: Symmetical
Tactile vocal fremitus
Tidal percussion
Percussion:
Dull note in 5th and 6th ICS
Resonant note in 5th ICS when he took deep breath.
Resonant note elsewhere .
Auscultation:
Breath sounds heard.
Cardiovascular system
S1 S2 heard No murmurs.
Central nervous system:
No focal neurological deficits,all cranial nerves intact .
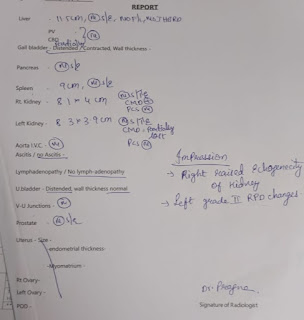
INVESTIGATIONS :
Ascitic fluid collected .
*PROVISIONAL DIAGNOSIS:
DECOMPENSATED LIVER DISEASE WITH ASCITES AND HEPATIC ENCEPHALOPATHY AND JAUNDICE .
TREATMENT:
1. FLUID RESTRICTION.
2. SALT RESTRICTED NORMAL DIET.
3. INJ. CEFOTAXIM 2 GRAM TWICE DAILY INTRAVENOUSLY.
4. INJ. VIT K 1 AMP IN 100 ML NS ONCE DAILY INTRAVENOUSLY.
5. INJ. THIAMINE 1 AMP IN 100 ML NS ONCE DAILY INTRAVENOUSLY.
6. INJ. PAN 40 MG TWICE DAILY INTRAVENOUSLY.
7. INJ. ZOFER 4 MG THRICE DAILY INTRAVENOUSLY.
8. TAB. PCM 650 mg SOS (<1 GRAM / DAY).
9. SYP. LACTULOSE 15 ML 30 MINUTES BEFORE FOOD THRICE DAILY.






.jpg)
















Comments
Post a Comment