70 year old male with dribbling of urine
This is an online e log book to discuss our patient de-identified health data shared after taking his / her / guardians signed informed consent. Here we discuss our individual patients problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problem with collective current best evident based input.
This E blog also reflects my patient centered online learning portfolio and your valuable inputs on the comment box is welcome.
I have been given this case to solve in an attempt to understand the topic of " patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations and come up with diagnosis and treatment plan.
*PRESENTING COMPLAINTS:
C/O Dribbling of urine since 10 days.
C/O Fever since 7 days.
C/O Myalgia since 5 days.
C/O Dry cough since 2 days.
*HOPI:
A 70 year male, labourer by occupation presented to the casuality with complaints of dribbling of urine since 10 days.
No history of dysuria/ burning micturition/ hematuria.
History of high grade Intermittent fever associated with chills releived on taking medication since 7 days. History of myalgia since 5 days and history of dry cough since 2 days.
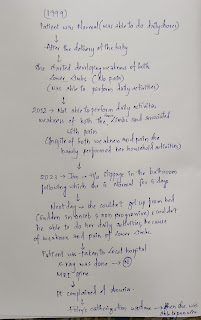
*PAST ILLNESS:
The patient had complaints of severe low back pain, paresthesia in the lower limbs and sough for consultation and underwent L-S spine fixation under GA in 2004, which was uneventful.
He was diagnosed with Diabetes Mellitus on regular health checkup which were conducted in the Health center; and started on Oral hypoglycemic agents since 2010.
History of loin pain radiating to the groin on the right side in the year 2017; Patient soughted for consultation for the same and treated conservatively.
*PERSONAL HISTORY:
Mixed diet
Sleep was adequate.
Appetite decreased.
Bowel and bladder are irregular.
Smoker: started at the age of 24 years and discontinued in the year 2004; he used to smoke 2 beedi's daily during initial years which progressed to 10 beedi's daily.
Occasional Alcoholic : started at the age of 26 years; 90ml/day; last binge was 12 days ago(90ml).
*GENERAL EXAMINATION:
Patient was conscious , coherent and cooperative Well built and nourished well oriented with time ,place and person
Pallor
Ictherus
Cyanosis
Clubbing
Pedal edema
Lymphadenopathy
Vitals
Febrile, Temp : 102°F.
PR: 102 bpm
RR: 19 cpm
BP: 110/80mmHg
GRBS: 247 mg/dl.
Systemic examination
CVS: S1, S2+
R/S: BAE+
P/A: Soft, Non tender, BS+, Hypogastric fullness+
CNS: NFND.
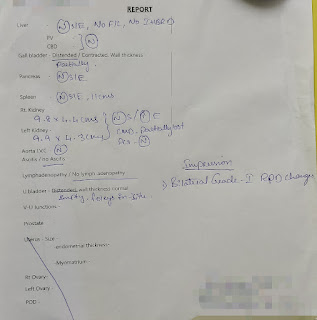
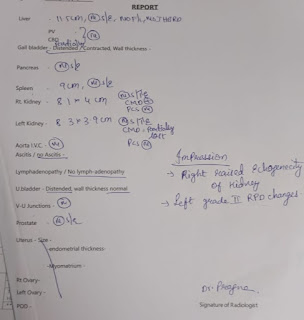
INVESTIGATIONS
Hb- 12.9
TLC-10,900
HbA1c-6.8
Blood urea -1.8
fever chart:



.jpg)








Comments
Post a Comment