19 year old male with fever and lower back pain
19 Year old male with fever and lower backache
December 01,2022
This is an online e log book to discuss our patient de-identified health data shared after taking his / her / guardians signed informed consent. Here we discuss our individual patients problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problem with collective current best evident based input.
This E blog also reflects my patient centered online learning portfolio and your valuable inputs on the comment box is welcome.
I have been given this case to solve in an attempt to understand the topic of " patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations and come up with diagnosis and treatment plan
This is a case of 19 year old male from mirylaguda who is intermediate second year student came to general medicine OPD with chief complaints of :
Fever since 4 days
Lower back ache since 4 days
Generalized weakness since 4 days
Abdominal pain since 4 days
HISTORY OF PRESENTING ILLNESS
Patient was apparently asymptomatic 10 days back then he developed high grade fever which was insidious in onset gradually progressive ,no diurnal variation which got relieved on medication given by local RMP [some IV medication was given for 1 day and oral medication is given].
Since 4 days he had high grade fever which was insidious in onset ,progressive and it is continuous not associated with chills and rigor ,no diurnal variation.
He had two episodes of vomiting 2 days ago which was non projectile contained food particles
He also complained of low back ache since 4 days which is insidious in onset ,gradually progressive, and is persistent and pain increased during inspiration and no relieving factors.[he was unable to describe the character of pain]
He also complained of abdominal pain which is insidious in onset persistent not associated with nausea and vomiting
He also complained of generalized weakness since 4 days
No history of burning micturition, increased frequency of urine ,difficulty to pass urine ,nocturnal eneursis
No history of loose stools
DAILY ROUTINE
He wakes up at 8 AM and does his morning routine , eats breakfast at 9 AM usually eats 4 idlies or 1 dosa or 4 bondas and goes to college at 9 AM by bus as his college is 10-25 km far from his home ,He is a CEC student attends all his classes and eat lunch at 2PM usually he eats junk foods [fried rice ,noodles,road side foods] almost daily as he feels embarrassed taking lunch box along with him , college ends at 4 PM ,comes back to home by 5 PM and eat dinner at 6 PM ,he usually prefers to eat rice in dinner. After having dinner he watches movies till 12 AM or go out with friends
His parents are agricultural labourer so sometimes he goes along with them Or sometimes he skips college and goes to work along with his cousin brother as part of recreation [ his cousin brother has plastic and iron shop where they store all the plastic and iron which they collected and sell them to others for reuse]
PAST HISTORY :
History of fever 10 days back which was diagnosed as typhoid and was given oral medication for 3 days and iv medication for 1 day
No history of Hypertension, diabetes, asthma, epilepsy,TB
No history of prolonged hospital stay
No history of previous surgeries
FAMILY HISTORY
No significant family history
PERSONAL HISTORY
Diet : mixed
Appetite: decreased since 4 days
Bowel and bladder:regular
Sleep:adequate
History of toddy and beer consumption occasionally
GENERAL EXAMINATION
Patient was conscious,coherent cooperative
Moderately build and moderately nourished
well oriented to time ,place and person
Pallor : no pallor,Lower palpebral congestion is seen
Icterus: absent
clubbing: absent
cyanosis: absent
Lymphadenopathy: absent
Edema : absent
VITALS:
Temp: febrile
BP: 110/80 mmHg supine position
PR- 90 bpm
RR- 16cpm
SYSTEM EXAMINATION:
Abdominal examination-
INSPECTION
On Inspection Abdomen is flat, no abdominal distension, umbilicus is central and inverted ,no engorged veins,no scars,sinuses,hernial ornifices are clear
PALPATION
All inspectory findings are confirmed
Tenderness present in epigastric region and right hypochondrium region
Tenderness present in right renal angle
Blanching present on Abdomen and back
liver dullness in 5th intercoastal space,
PERCUSSION : No significant findings
AUSCULTATION: bowel sounds heard
RESPIRATORY EXAMINATION
trachea central,
normal respiratory movements,
normal vesicular breath sounds.
CARDIOVASCULAR SYSTEM
S1 ,S2 heard ,no murmurs
CNS EXAMINATION
No focal neurological deficits
INVESTIGATIONS
FEVER CHART
CHEST X-RAY
Date 29 Nov 2022
NS 1 antigen
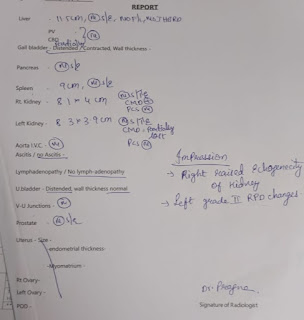
USG
Review USG on 30 Nov 2022
ECHO
On 1st December
*PLATELET TRANSFUSION IS DONE :
PROVISIONAL DIAGNOSIS
*Dengue fever
*serositis
TREATMENT
On 29 Nov 2022
1.IVF- NS/RL @75ml/hr
2.INJ PANTOP 40mg/IV/OD
3.TAB DOLO 650mg/PO/TID
4.TAB ZOFER 4mg/PO/SOS
5.INJ NEOMOL 100ml
On 30 Nov 2022
1.IVF- NS/RL @75ml/hr
2.INJ PANTOP 40mg/IV/OD
3.TAB DOLO 650mg/PO/TID
4.TAB ZOFER 4mg/PO/SOS
5.INJ NEOMOL 100ml
On 1st Nov 2022
1. IVF- NS/RL @100ml/hr
2. INJ PANTOP 40mg/IV/OD
3. TAB DOLO 650mg/PO/TID
4. TAB ZOFER 4mg/PO/TID
5. INJ NEOMOL 100ml/IV/SOS
6. PIPTAZ 4.5g/IV/TID























Comments
Post a Comment