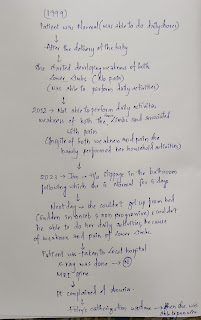
48 year old male with chronic kidney disease secondary to heart failure
48 year old Male came to the medicine OPD with chief complaints of
Difficulty in breathing since 5 days
Decreased urinary output since 3 days
Swelling of lower limbs since 1 year
HISTORY OF PRESENTING ILLNESS
Patient was apparently asymptomatic 1 year back then he developed bilateral pedal edema which is insidious in onset gradually progressive, from knee to ankle region, and was on conservative treatment. He went to local hospital for swelling of limbs and was diagnosed with hypertension and started using medication (drug-Telmisartan dosage-40mg)since 1 year.
5 days before at night the patient developed shortness of breath which is sudden in onset and gradually progressive which is of class 3, associated with orthopnea and paroxysmal nocturnal dyspnea
Decreased urinary output and it is of streamlined urine since 3 days
History of intermittent fever not associated with chills and rigor
not associated with chest pain , palpitations , sweating
No history of burning micturition
No history of jaundice, parotid swelling, abdominal distension,dilated abdominal veins
DAILY ROUTINE
Patient wakes up at 5:30 in the morning and does his household chores and goes to work daily work for about 5 hours and comes back between 12-1 pm to have lunch, and takes rest for the day. Patient have dinner at around 7:30 in evening and goes to sleep at 9pm.
PAST HISTORY
Known case of hypertension since 1 year
No similar complaints in the past
Not a known case of DM, asthma, epilepsy, thyroid disorders.
DRUG HISTORY
Started using Telmisartan 40 mg since 1yr
FAMILY HISTORY
No similar complaints in the family
PERSONAL HISTORY
Appetite - Normal
Diet - mixed
Sleep - Adequate
Bowel and bladder -Regular, Decreased micturition
Addictions :Smoking history (4 beedis per day so 6 pack years)
Alcohol history -since 25 years 4 times monthly(whisky 90 ml each time)
GENERAL EXAMINATION
Patient is consious, coherent, and cooperative
moderately built and moderately nourished
Pallor - present
Icterus-absent
Cyanosis - absent
Clubbing-absent
Lymphadenopathy -absent
Pedal edema -present( grade 1 upto ankle )
vitals
Temperature - Afebrile
Pulse - 76 bpm
Blood pressure- 130/80 mmhg
Respiratory rate- 17 cycles per min
Spo2 - 95%
SYSTEMIC EXAMINATION
CVS-
Inspection
No palpitations
JVP seen
Palpation
Apex beat is felt at 6th intercoastal space
No parasternal heave
Auscultation:
S1 S2 heard
RESPIRATORY SYSTEM
No scars, pulsation, engorged veins.
chest is bilaterally symmetrical
shape of chest - elliptical
Bilateral air entry present
Trachea - Midline
A crested healing ulcer is seen on anterior aspect of right hemithorax medical to the nipple
Percussion-
right left
supra clavicular resonant resonant
infra clavicular resonant resonant
supra mammary resonant resonant
infra mammary resonant resonant
axillary resonant resonant
supra axillary resonant resonant
infra axillary resonant resonant
supra scapular resonant resonant
infra scapular resonant resonant
Auscultation:
b/l wheeze present in mammary, inframammary
Crepts present in b/l inframammary areas
ABDOMINAL EXAMINATION
shape- scaphoid
No tenderness
no palpable mass
liver not palpable
spleen not palpable
CNS EXAMINATION
speech normal
no focal neurological deficits seen
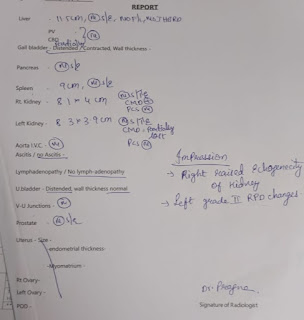
INVESTIGATIONS
Complete blood picture
hemoglobin - 8.6 gm/dl
total count - 19,200cells/cumm
neutrophils - 91%
lymphocytes - 3%
pcv - 27.6%
blood group A+
interpretation- Normocytic normochromic anemia with neutrophilic leukocytosis
URINE EXAMINATION
albumin ++
sugar nil
pus cells 2-3
epithelial cells 2-3
Red blood cells 4-5
random blood sugar - 124 mg/dl
Renal functional test
urea 154/dl
creatinine 5.9mg/dl
uric acid 8.7 mg/dl
sodium 133mEq/L
Serum Iron- 74 ug/dl
Liver functional test
Alkaline phosphate 312 mg/dl
total protein 6.2 gm/dl
albumin 3.04gm/dl
ABG ANALYSIS
pH - 7.13
pCO2 - 34.1 mmHg
pO2 - 54.6 mmHg
HCO3 -11.1 mmol/L
O2 saturation 95.9%
ECG:
X-ray :
X ray findings:
-Cardiomegaly
- b/l perihilar bronchovesicular prominence
-straightening of the left heart border
- haziness at right lower zone
Multiple ulcers can be seen at the back of the body.










Comments
Post a Comment